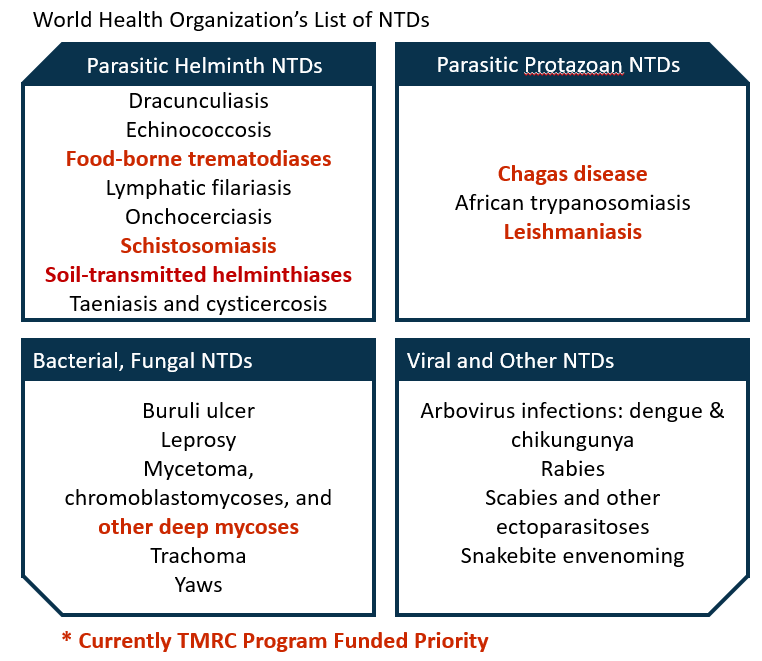
Neglected Tropical Diseases
Neglected tropical diseases (NTDs) are most prevalent in tropical areas with their greatest effect being on impoverished communities and disproportionately affect women and children. Over 1.6 billion individuals are impacted by NTDs.
NTDs are transmitted via a variety of sources with many being related to environmental conditions, being vector-borne, having animal reservoirs, and complex life cycles. The factors complicate public-health control.
Chagas disease
Chagas disease, also referred to as American trypanosomiasis. is caused by the parasite Trypanosoma cruzi (T. cruzi). Infection is lifelong without treatment and can be life threatening. Chagas disease is found in the Americas.
Chagas disease is transmitted by insect vectors known as triatomine bugs to both humans and animals. The triatomine bugs, also referred to as “kissing bugs,” are found in house materials such as mud, adobe, straw, and palm thatch and emerge at night to bite sleeping people’s faces. T. cruzi parasites are transmitted by the sleeping person scratching or rubbing the bug’s feces into open wounds or orifices.
During the first several weeks or months after the infection, individuals may be completely asymptomatic or only have mild symptoms that are common to many other illnesses including fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. The subsequent chronic phase can last for decades or be lifelong and is usually symptom free; however, 20-30% percent of infected individuals do develop more severe cardiac and/or gastrointestinal complications.
Therapeutic options include treatment to kill the parasites and treatment of the infection symptoms.
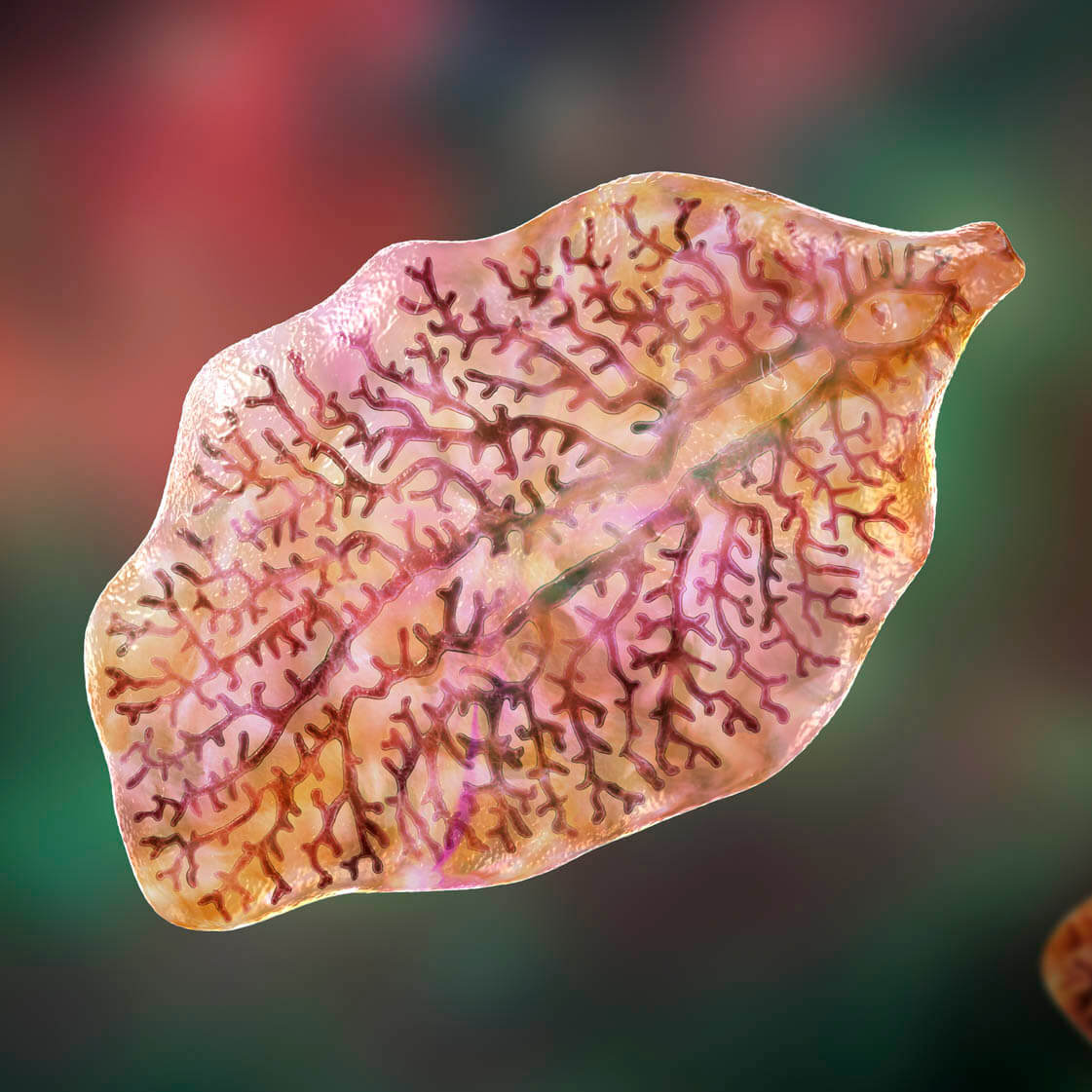
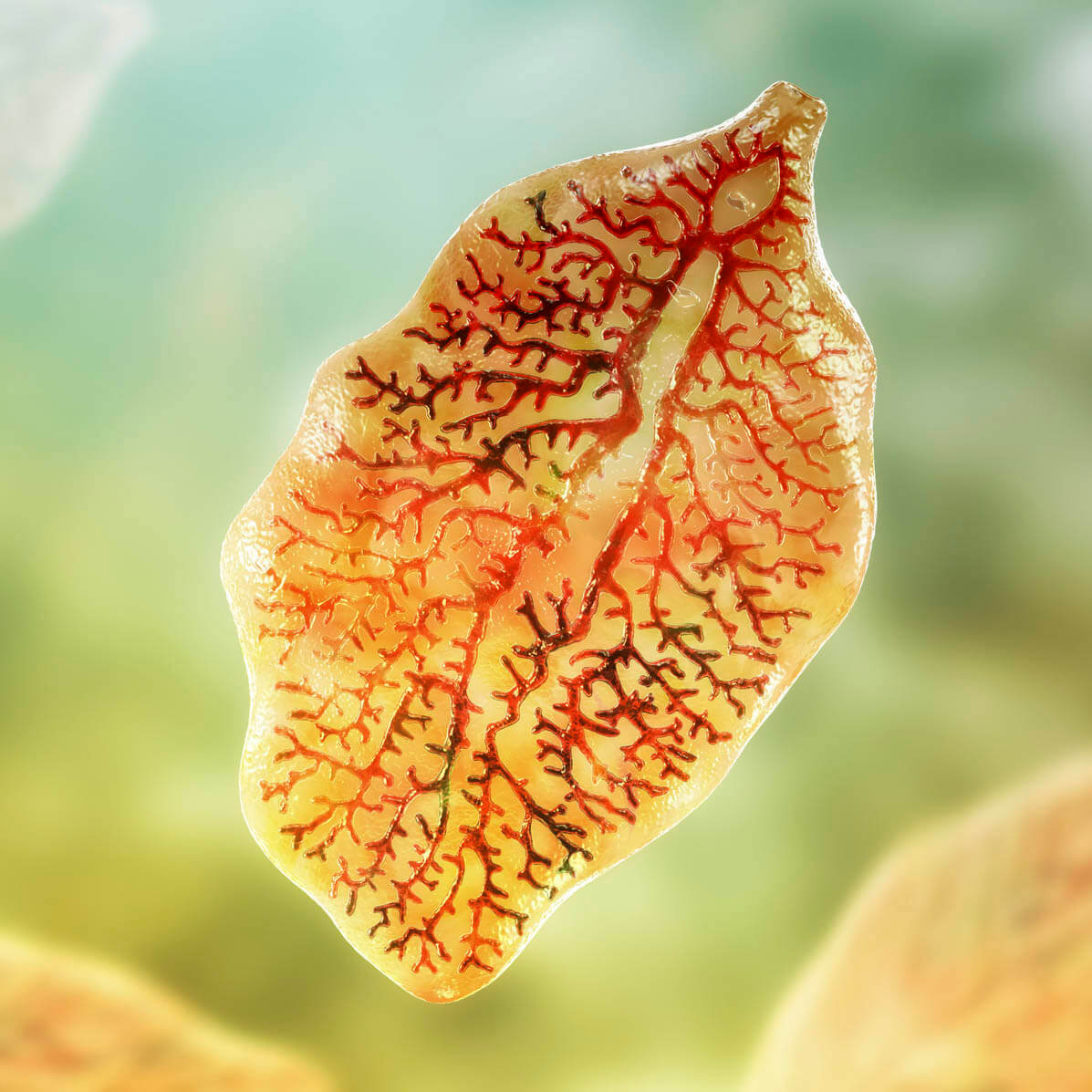
Food-borne trematodiases: Fascioliasis
Fascioliasis is caused Fasciola parasites, which are flat worms also known as liver flukes. Fascioliasis is found in more than 50 countries.
While fascioliasis is more common in animals, particularly livestock, than in people, two Fasciola species infect people including Fasciola hepatica, also referred to as “the common liver fluke” and “the sheep liver fluke,” and Fasciola gigantica. Infection primarily occurs by ingesting the parasite through eating raw watercress or other contaminated freshwater plants or drinking or cooking with contaminated water.
During the first several weeks or months after the infection, individuals may be completely asymptomatic or only have mild symptoms that are common to many other illnesses including fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. The subsequent chronic phase can last for decades or be lifelong and is usually symptom free; however, 20-30% percent of infected individuals do develop more severe cardiac and/or gastrointestinal complications.
Therapeutic options include treatment to kill the parasites and treatment of the infection symptoms.
Schistosomiasis
Schistosomiasis, also referred to as bilharzia, is caused by parasitic worms. Schistosomiasis is most prevalent in tropical and subtropical areas with at least 90% of those requiring treatment living in Africa.
Disease in humans is most commonly caused by Schistosoma mansoni, S. haematobium, and S. japonicum and less commonly by S. mekongi and S. intercalatum. Infection primarily occurs due to individual’s skin exposure to freshwater contaminated by snails carrying schistosomes (i.e., through wading, swimming, bathing or washing).
Symptoms of a rash or itch skin may start within days after becoming infected; however, most individuals are asymptomatic during the acute phase. Symptoms within two months of infection can also include fever, chills, cough, and muscle aches. During the subsequent chronic phase, liver, intestine, lungs, and bladder damage and more rarely seizures, paralysis, or spinal cord inflammation can occur.
Therapeutic options include multiple safe and effective drugs such as praziquantel.
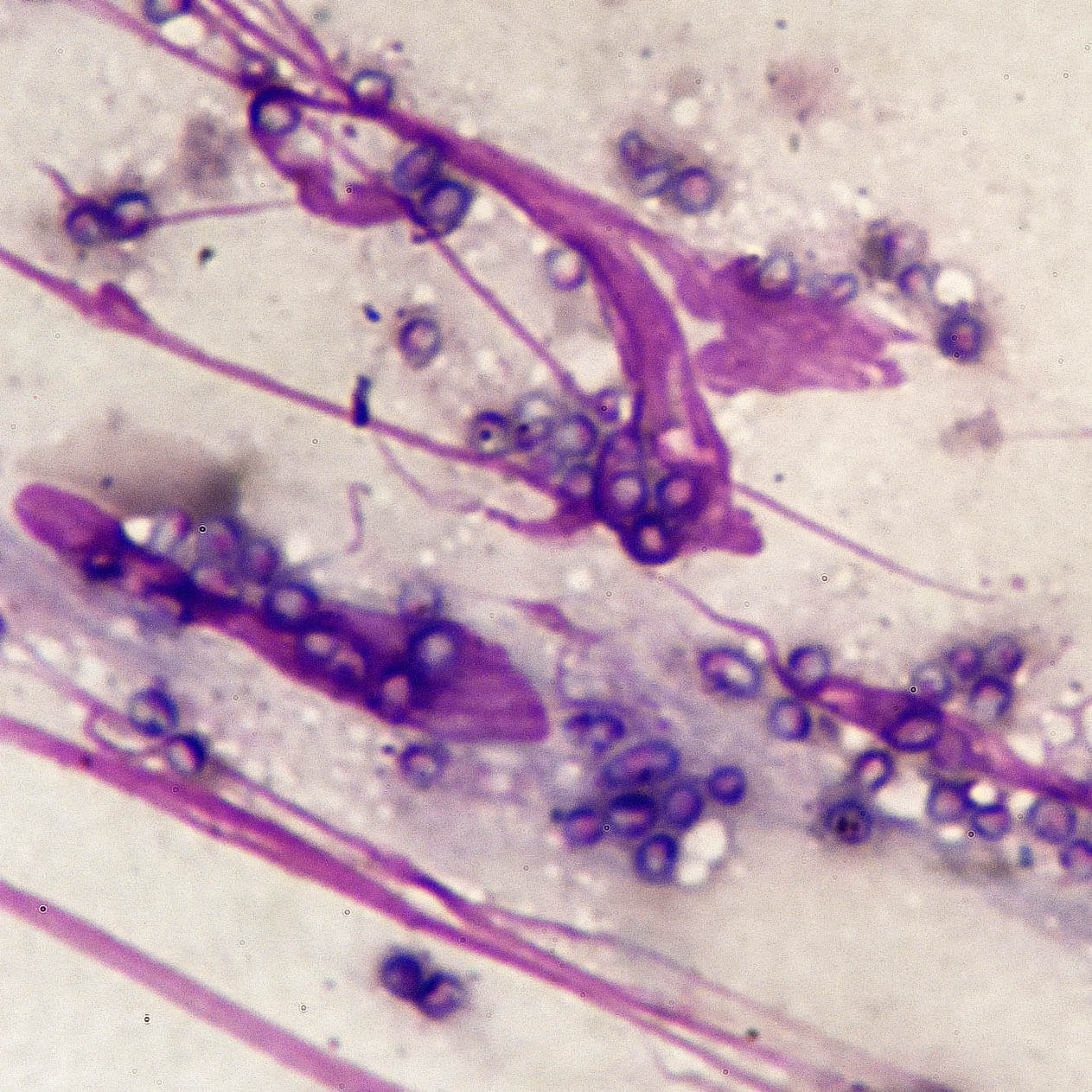
Deep Mycoses: Talaromycosis
Talaromycosis is caused by the fungus Talaromyces marneffei. Talaromycosis is found in Southeast Asia, southern China, and eastern India.
Disease most commonly occurs in individuals with weakened immune systems including those with HIV/AIDS. While the environmental source of talaromycosis is unknown, scientists hypothesize that infection occurs by breathing in T. marneffei from the environment.
Early symptoms include fever, weight loss, hepatosplenomegaly, lymphadenopathy, and respiratory and gastrointestinal abnormalities. During the subsequent chronic phase, skin lesions are common including central-necrotic papules appearing on the face, trunk, and extremities. Other symptoms include cough or shortness of breath, diarrhea or abdominal pain, as well as abdominal distention and pain. Less common is meningoencephalitis which can lead to death.
Therapeutic options include treatment with prescription antifungal medicine, most commonly amphotericin B followed by itraconazole. Other options include voriconazole or itraconazole alone.
Visceral leishmaniasis, PKDL
Leishmaniasis is caused by Leishmania parasites. It is most prevalent in Brazil, East Africa and in India with greater than 90% of new cases in 2020 occurring in 10 countries: Brazil, China, Ethiopia, Eritrea, India, Kenya, Somalia, South Sudan, Sudan and Yemen.
Disease occurs via transmitted through the bites of infected female phlebotomine sandflies, which feed on blood to produce eggs. Over 70 animal species, including humans, are natural reservoir hosts of Leishmania parasites.
Symptoms of visceral leishmaniasis (VL), also referred to as kala-azar, include irregular bouts of fever, weight loss, enlargement of the spleen and liver, and anemia. VL can is almost always fatal if left untreated. Post-kala-azar dermal leishmaniasis (PKDL) commonly follows six to twelve months after VL has been cured with symptoms of macular, papular or nodular rash usually on face, upper arms, trunks and other parts of the body.
Therapeutic options exist for various forms of leishmaniasis but do require an immunocompetent system as treatments do not get rid of the parasite and therefore relapse is possible.
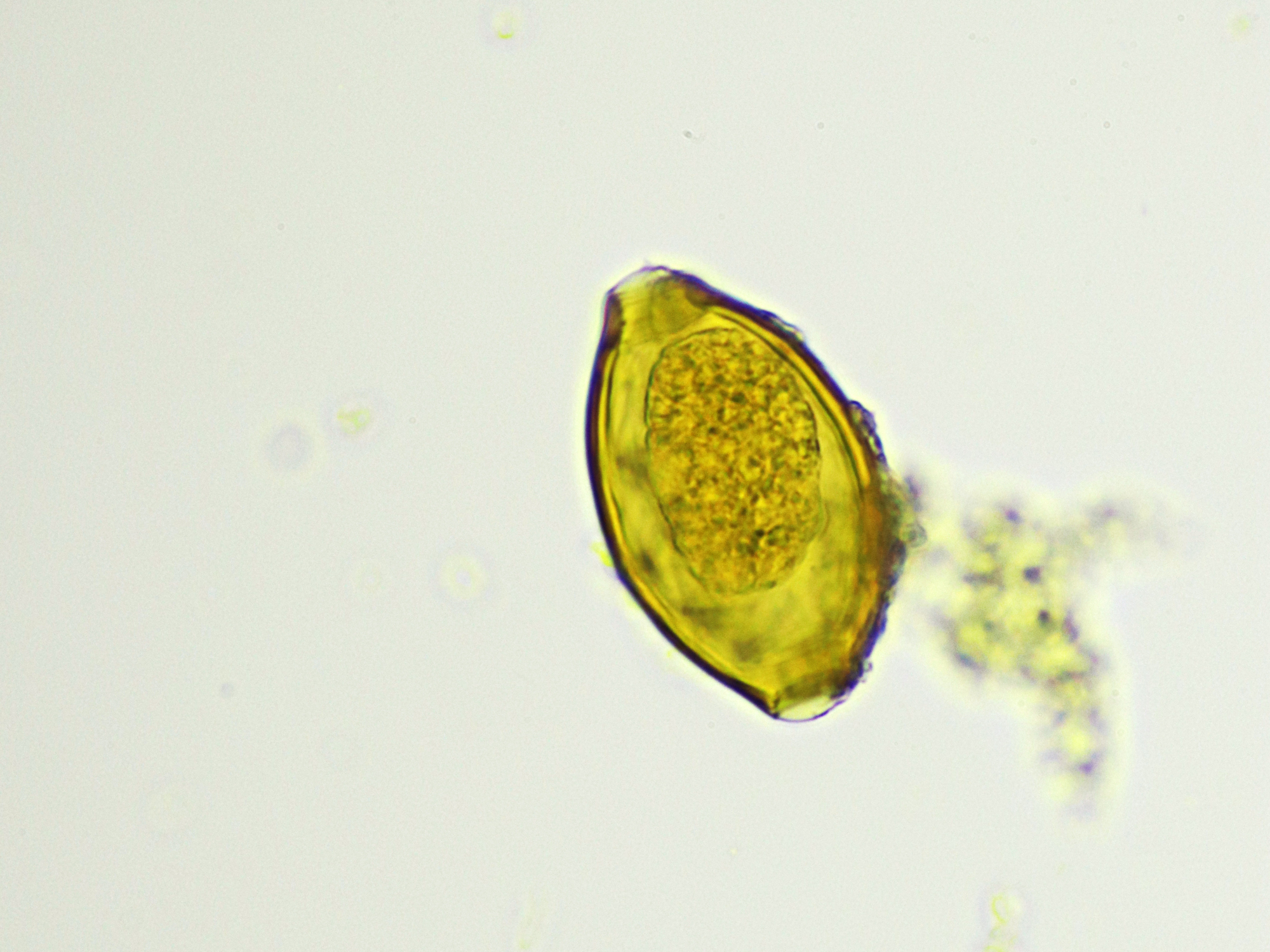
Soil-transmitted helminths (STH)
Soil-transmitted helminth (STH) infections are caused by intestinal worms. These infections are found primarily in warm and humid climates with poorer sanitation and hygiene such as sub-Saharan Africa, China, South America and Asia.
Disease occurs via transmission through eggs present in human feces in turn contaminating the soil. The primary species that infect humans include roundworm (Ascaris lumbricoides), whipworm (Trichuris trichiura) and hookworms (Necator americanus and Ancylostoma duodenale).
Mild infections are typically asymptomatic. Symptoms of more severe infections include intestinal manifestations (diarrhea and abdominal pain), malnutrition, general malaise and weakness, and impaired growth and physical development. Severe infections can lead to intestinal obstruction that requires surgery.
Therapeutic options include albendazole, mebendazole, and ivermectin.